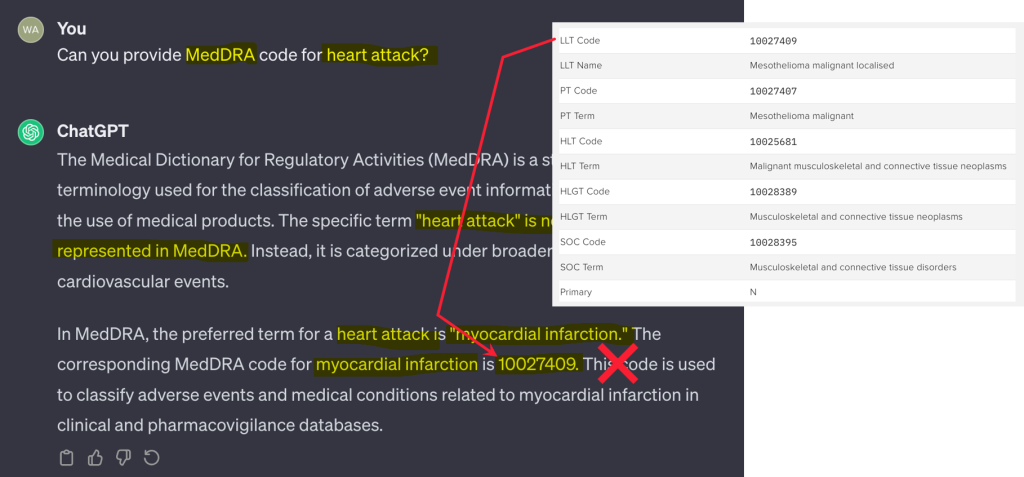
Will DCTs finally democratize clinical trials?


Walker Bradham
Sr. Dir. Product Management & Design, Zelta by Merative

Wes Fishburne
Senior Product Manager, Merative
Zelta Product Leader Walker Bradham and Senior Product Manager Wes Fishburne discuss the patient experience in centralized clinical trials.
Finding a cure for a disease is a long road, and perhaps no one appreciates that more than the clinical trial participants who help discover those cures. According to industry estimates, the average clinical trial patient travels between 50 and 100 miles to reach a clinical site — and even farther in the case of rare or serious diseases. But not every patient has the drive that it takes to make that journey. The healthcare industry understands that clinical trials need to be more inclusive in terms of accommodating patients who live far away or can’t take off work to visit a clinical site. Which begs the question, is decentralization the answer to finally democratizing clinical trials?
It's hard not to get excited about the potential for decentralized clinical trials (DCTs). Who wouldn’t rather wear a smartwatch than drive 75 miles to have someone measure their blood pressure? And trial sponsors themselves have a reason to be excited, too. Instead of collecting random samples and reports every three or six weeks, clinical research organizations (CROs) can have a steady stream of self-reported data coming in for analysis and outcome assessment through DCT technology.
DCTs Open the Door to More People
For years, the healthcare industry has recognized the need to expand clinical trial populations to include more people from a broader range of demographics. Currently, clinical trials are often limited to people who live close to the testing facility and are available to visit the testing site multiple times. As a result, individuals who live in rural regions or who may be unable to take time off from work and family responsibilities to visit a testing facility are unintentionally, but inevitably, excluded from participating in clinical trials.
DCTs offer the potential to expand the participant population by decentralizing many of the facility-based functions through Internet-based access, televisits, wearable devices, remote reporting and other digital technologies. With the unexpected arrival of the Covid pandemic in 2020, many CROs began to adopt DCT technologies by necessity. With healthcare organizations overwhelmed and non-essential medical visits restricted, DCT technologies such as electronic consent (eConsent), electronic patient-reported outcomes (ePRO) and electronic clinical outcome assessments (eCOA) allowed CROs to continue clinical trials remotely. Now, with many of those Covid-era restrictions lifted, it remains to be seen what role DCT technologies will play in the future.
Understanding the Risk of Remotely Collected Data
While everyone can agree that making patients feel comfortable is essential to a successful trial, finding a consensus among patients of what constitutes “comfort” is more elusive. For younger patients, using an app on their iPhone to log in daily journal entries may be second nature. For older patients or those already situated in a healthcare facility, face-to-face meetings are likely to be more comfortable.
The same challenges exist when discussing wearable devices. Some patients may be very good about wearing devices at the prescribed times. Others may be less disciplined. And this raises an important issue for data that is collected remotely: How can CROs trust that self-reported data is accurate? Because many clinical trials are seeking FDA and other regulatory approval, there are strict requirements around data quality and integrity. By contrast, most mobile devices (including wearables and smartphones) aren’t certified for clinical trials. And so CROs need to be careful about how they collect and use DCT data sources like these in their trials.
Are DCTs the Future of Clinical Trials?
There’s no question that decentralizing clinical trial processes has significant upside for patients and trial sponsors. It can bring a broader sample of the general population into trials, reduce the burden of traveling to site facilities for testing and reporting, reduce trial costs, generate better data for analysis and ultimately accelerate the discovery and development of new treatments. But none of these goals should be pursued at the exclusion of making all patients feel comfortable with the trial experience.
Decentralization shouldn’t be an all-or-nothing approach. Rather, CROs should take a hybrid approach that provides comfortable alternatives for all patients. For some trials, this will mean offering a mix of self-reporting and site reporting options. While tools such as eConsent may be familiar to everyone, logging onto an ePRO app may be confusing for some patients. And even for patients who are comfortable with digital devices, they may prefer to use their own devices rather than be given a device by the CRO for the trial duration.
This need for flexibility must be balanced with repeatability — that is, the ability to create repeatable processes that can be re-used for multiple trials. Without that, trial costs and complexity will escalate and the benefits of DCT technology will effectively be neutralized. At Zelta ™, our focus is on creating repeatable and reliable trials that mix and match the best of traditional and decentralized trial tools to deliver the best patient experience. And, when you think about it, isn’t making patients feel better what clinical trials are all about?
Merative Clinical Development was renamed Zelta in February 2023. More information can be found here.
Related Articles
How supervised machine learning optimizes AI use in clinical trials
LLMs are frequently hailed as revolutionary tools in clinical trials. Read how...
By Walker Bradham | 5 min. read
Let the use case decide: The Zelta way on AI and supervised machine learning
For decades, when people thought of artificial intelligence (AI) what usually...
By Walker Bradham | 2 min. read

Clinical trial trends in 2025: Investment headwinds, wearables, and targeted AI uses
This article originally appeared on Pharmaceutical Technology.2025 is set to be...
By Jennifer Duff | 7 min. read
Ready for a consultation?
Our team is ready to answer your questions. Let's make smarter health ecosystems, together.